The 4 Stages of Patient Engagement and the Patient's Role in Self-Management
At 63 years old, Lucas had been living with a diagnosis of heart failure for over a decade. To control his condition, he was taking beta blockers and antihyperintensive drugs on a daily basis. Yet in spite of this regimen, he was diagnosed with advanced heart failure.
Medical professionals encounter patients with serious health diagnoses like Lucas on a regular basis. Along the way, they’ve probably noticed that each patient reacts very differently when learning of a life-threatening condition. For instance, some patients go into denial, whereas others quickly assess the risks so they feel empowered to make medical decisions.
Until recently, there has been no straightforward methodology for evaluating this type of patient engagement, or lack thereof. Fortunately, today we have the Patient Health Engagement (PHE) Model developed by Guendalina Graffigna.
Guendalina Graffigna, an organisational psychologist based in Italy, began her career focusing on the dynamics of consumer brand engagement—essentially, what makes people get involved with some brands and not others. During this time, she also completed a PhD in health promotion and behaviour change where she researched AIDS prevention and how social communication affects HIV risk.
As a result of her studies, Graffigna realised her passion for health care and transferred her understanding of brand engagement to patient engagement. She quickly discovered there was a lack of understanding of the psychological factors influencing patient engagement and performed research to develop the PHE Model.
The PHE Model
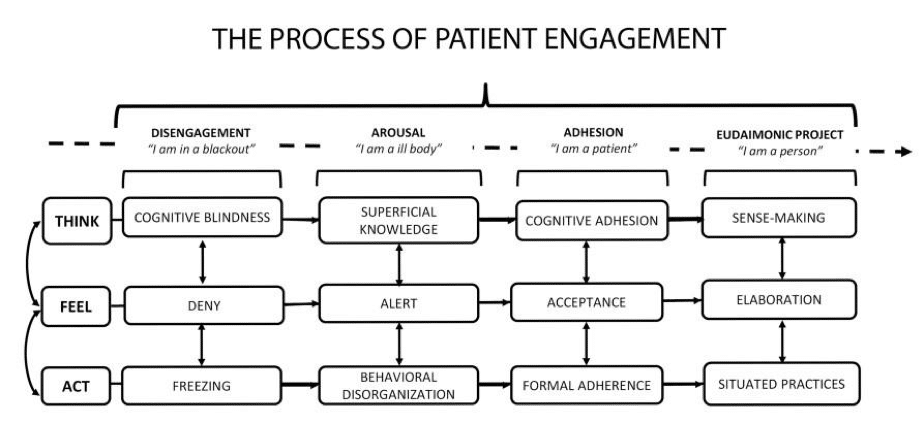
The Patient Health Engagement Model is a psychological framework that depicts four phases or emotional positions that patients can pass along on their healthcare pathway.
The basic concept of the model is that the patient needs to change their perception of their own identity to transition from a passive role to an active role.
In essence, if there isn’t a change in how patients look at themselves and their disease after their diagnosis, then they typically lack the strength and motivation to play an active role in self-management.
The PHE Scale
From this model the PHE Scale, which stands for ‘Patient Health Engagement Scale’ is derived. The PHE Scale is a psychometric scale designed to be easily used by clinicians during consultation with a patient. Although the scale can be answered by patients themselves, it presents an excellent opportunity for doctors or nurses to further the patient-provider relationship.
The scale includes 5 points where patients can position themselves. Patients can decide where they feel they are positioned by reviewing the scenarios described. A simple algorithm then turns these answers into a score.
Source: Consortium for Patient Engagement, 2015
Disengagement Stage
For instance, a patient in the disengagement stage would be one that’s much like Jim.
Jim’s 77 years old, and he’s been living with heart failure for three years. He also has ulcerous colitis. Recently he was diagnosed with early-stage prostate cancer. Because nobody in his family has any previous experience with this disease, Jim’s shocked, scared, and uncertain. Although he’s consulted with a urologic surgeon and a radiation oncologist, Jim feels overwhelmed by his treatment options and unable to make a sound decision.
Arousal Stage
Compare Jim’s experience to that of a patient in the arousal stage.
Maria, a 68 year old woman diagnosed with osteoporosis feels worried about her health (FEEL), lacks confidence in the information her physician shared with her about the disease (THINK), and doesn’t believe she can autonomously manage the medical regimen of physical rehabilitation she was prescribed (ACT).
Although Maria was given an at-home health platform called Health Platform that records environmental, movement, and bio-signals like health rate to help her manage her disease, her mindset prevents it from being as useful as it could be. She reports, “… I was only there, and I did the exercises but I have no idea, I am totally incompetent…”
Adhesion Stage
Moving up the PHE Scale, medical professionals are more apt to see a patient much like Janet.
Janet is a 55 year old overweight woman with high blood pressure and a 2-year diagnosis of type 2 diabetes mellitus. Janet’s doctors have told her that she either needs to take more medication or lose weight and exercise more, which may prevent the need for increased medication.
Although Janet is ambivalent about making any lifestyle changes, she can still be said to be in the Adhesion phase of the PHE model, because she understands clinical information about her disease, and is able to face discussions about treatment, care expectations, symptoms, and health monitoring. She expects her doctors—as experts—to help her when it comes to making decisions about medical treatment.
Eudaimonic Project Stage
The final phase of patient engagement is known as the eudaimonic project stage. In this phase, patients are totally aware of their condition and its risks. After discussing their priorities with their clinicians, they feel empowered to make final treatment decisions. This is known as shared decision making, because patients reach a decision in conjunction with their physicians, rather than deferring those decisions to medical professionals.
PHE Scale Usage
Although the PHE Scale originated in Italy, today it’s used around the world in multiple ways. For instance, Graffigna’s team is now designing personalised counseling procedures and exercises, based on patients’ levels of engagement. These procedures have been published and trials have already started in Italy.
When asked how the trials are going, Graffigna said, “In Italy both nurses and doctors are very happy because they say they finally have an instrument to objectify their interpretation of their patients. Because sometimes you have practitioners who are at the beginning of their career, or perhaps are less empathetic by personality, so it’s really hard to correctly diagnose every time on such a subjective matter, especially because they are not trained to communicate about emotions.”
So, the scale is a way to measure, assess and gather more objective data on a very subjective matter, but on the other hand, is very therapeutic because it opens a space where patients feel legitimised and able to express their very inner needs because they are able to touch on and express very deep problems.
Another application of the scale is for medical communication—essentially, to determine the best communication strategies a healthcare professional can use with patients, based on their self-selected position on the PHE scale. This not only helps patients become more aware of their situation, but also gets them more involved in the process of recovery.
How can I get started?
To use the scale properly, Graffigna says that medical professionals need to first be trained on how to use the tool to decode the results. After this training, the results are very straightforward; in just a few minutes of using the test, practitioners can understand how to best move forward with a patient.
In exchange for free access to the scale, Graffigna and her team request that any data gathered be shared with them so they can improve the model.
You can read the full Patient Engagement publication for free here: www.degruyter.com/view/product/466090
Alternatively, you can learn more about the consumer and health engagement research center, Engageminds-HUB, by visiting www.engagemindshub.com/
In Conclusion
Because patient engagement has such a significant impact on treatment outcomes, understanding it better is critically important for healthcare providers. That’s why the Patient Engagement Model is so valuable.
Clearly, we can see this when we look at a patient like Lucas, the 63 year old man mentioned at the beginning of this article. Because he was diagnosed with advanced heart failure, he was advised of two treatment options: therapies to reduce the risk of sudden cardiac death like ICD and advanced surgical therapies like transplantation.
Lucas feels knowledgeable about his condition, well-informed of the risks, and understands the pros and cons of the various therapies. You could say that he’s in the eudaimonic project phase, which is characterised by empowerment and a shared decision making style.
This positive approach—and active role in decision-making—should be the goal for all patients. While medical professionals can’t force them to adopt that mindset, they can further it along with a better understanding of the Patient Engagement Model and its various stages.


