Earlier this week we published an article: Why is Australia So Bad at Preventative Health? The piece revealed just how poor Australia is when it comes to preventing chronic disease and reducing the burden placed on our hospitals. Not that this is the fault of any individual doctor or primary care worker. Most want nothing more than to put a dent in preventative health. The trouble is how?
The current landscape
It seems everything is against primary care workers when it comes to bettering our approach to preventative disease: there are very few Medicare items available for preventative activities; these items are very restrictive; those most in need of support are the ones least engaged with the medical community; and the general mantra among Australians is that the doc is there when I get sick, not before.
This paints a pretty drab picture about what a primary care worker can do to make change. It doesn’t have to be though because the good news is change is in motion. Slowly the general population is becoming more conscious of their health and the importance of preventative care. As a community we’re evolving towards a more ‘health prevention’ focused mindset. Not just in a ‘I want to lose weight’ way but in a ‘I want to nourish my body’ way.
Whether you want to credit influencers (athletes, actors, podcasters etc) who are obsessed with their health, the pressures of social media, or just the general access to more information, there is hope for the future of preventative health in Australia.
This said, of course, we still have some way to go. One day we’ll more than likely have laboratories connected to our toilets that collect stool samples daily and tell us what we’re missing from our diet. We’ll have devices that track every movement of our body and deliver intel on how to exercise and when to rest. And we’ll replace organs likely to fail well before they get a chance to.
For now it’s baby steps, but those who will ultimately determine the speed of this change are primary care workers. These people are the real merchants of change. Their views and actions will shift our communities like no other. But how exactly can they help? Well, here are our top 5 tips.
1. Don’t give up
The best thing a primary care clinician can do right now is not be discouraged. If you’re trying to put in place a health promotion or prevention activity and you’re not getting the uptake you hoped for, keep going. See these first attempts as education and awareness. Sometimes it will take years of reach outs before a patient finally decides to take action.
For instance, maybe you reach out to a patient when they are 40 years old for the 40+ health assessment. They ignore you. You try again at 41. They ignore you again. 42. Nothing. Then at 43 years old the patient finally says, ‘Okay, I’ll get the assessment. Obviously it’s important, otherwise they would have stopped contacting me.’
Start to view every interaction as planting the seeds of change.
2. Educate yourself as a clinician
The more educated you are about preventative health, the more help you can be to your patients because every little interaction you have will naturally promote the benefits of preventative care. For instance, being aware of the things you want to be screening for and the things that increase risks, or learning about behaviour modification and how you can support patients through behaviour change.
So even if you’re not doing an entire campaign about a certain health promotion, you’re at least peppering in preventative health messages when talking to your patients. This will plant the seeds in many patients and encourage them to be more conscious of preventative health.
The best way to educate yourself is to identify those things you don’t know much about and then seek out CPD modules to fill the gaps.
3. Form better relationships with allied health
Develop genuine relationships with other health workers like allied health. What tends to happen is that we have a token relationship with other healthcare workers—we send them patients and receive reports in return—but that’s it. We encourage you to go one step further and to develop an actual relationship with those from other fields.
Ask your allied health referrals why they do certain things the way they do them and what the evidence shows. Not only is this a great opportunity to learn something new but it will also more than likely help improve patient outcomes because it’s always more powerful when the same recommendations are being voiced by multiple parties.
4. Encourage patients to use health apps
Health apps are a great way for patients to manage their health and wellbeing between visits to the doctor. Of course, the hardest thing is knowing which apps to trust and which to avoid. The good news is that thanks to The Digital Health Guide you don’t have to guess. The platform helps clinicians safely and appropriately recommend mobile health apps to their patients. You may even find that your PHN has already purchased a subscription to the platform and that you already have free access.
5. Create a community of preventative health promotion
Another way to improve preventative health outcomes in your community is to think about what grassroots skills someone needs in order to achieve their goals. For instance, Dr Mukesh Haikerwal from Circle Health set up an entire floor to run cooking classes at his clinic because he knew that in order for people to get healthier and stop eating so much fast food they needed to learn how to cook.
Read our article: When the Recipe is the Remedy: A Conversation With Dr Mukesh Haikerwal
If you’re like most practices and running your own courses is unrealistic, we recommend you reach out to your local council instead. A lot of times there are great community programs that help with preventative health. Many of these programs simply struggle to get the word out. Why not help them get the word out, while at the same time using their resources to better support your patients?
Remember these programs aren’t just limited to diet and exercise. There are many great social prescribing programs too. These include gardening groups, art therapy groups, pet groups etc that all focus on integrating people back into the community. These can have a profound effect on people’s mental health, which often leads to improved physical health.
Read our article: Using ‘Social Prescribing’ to Improve Mental Health
6. Practice what you preach
It makes it very difficult for a patient to take advice from a clinician who doesn’t come across as practicing what they preach, or at least attempting to. On the flip side, a clinician who has gone through their own health transformation and can relate to the challenges a patient is facing when trying out a new healthy habit can be very influential.
7. Be patient
The final tip is to be patient and resist the temptation to give into frustration if things don’t progress as quickly as you would like. Meaningful lifestyle changes hardly happen overnight—they take time because barriers are often deeply rooted in a person’s psyche. It’s not enough for a patient to want to change, they have to believe they can and this often involves overcoming subconscious emotional attachments to their sense of self. The fact is, our habits become our identity, which means to change our habits we have to change the way we see ourselves and this is hard.
Remind yourself often that creating and sticking to healthy habits is a lifetime journey for most, and never underestimate the impact that genuine support and encouragement from a caring health professional can have on a patient. After all, to believe in ourselves, first we need others to believe in us—especially those we look up to—and who doesn’t look up to a clinician who truly cares?
HotDoc’s tool for preventative health
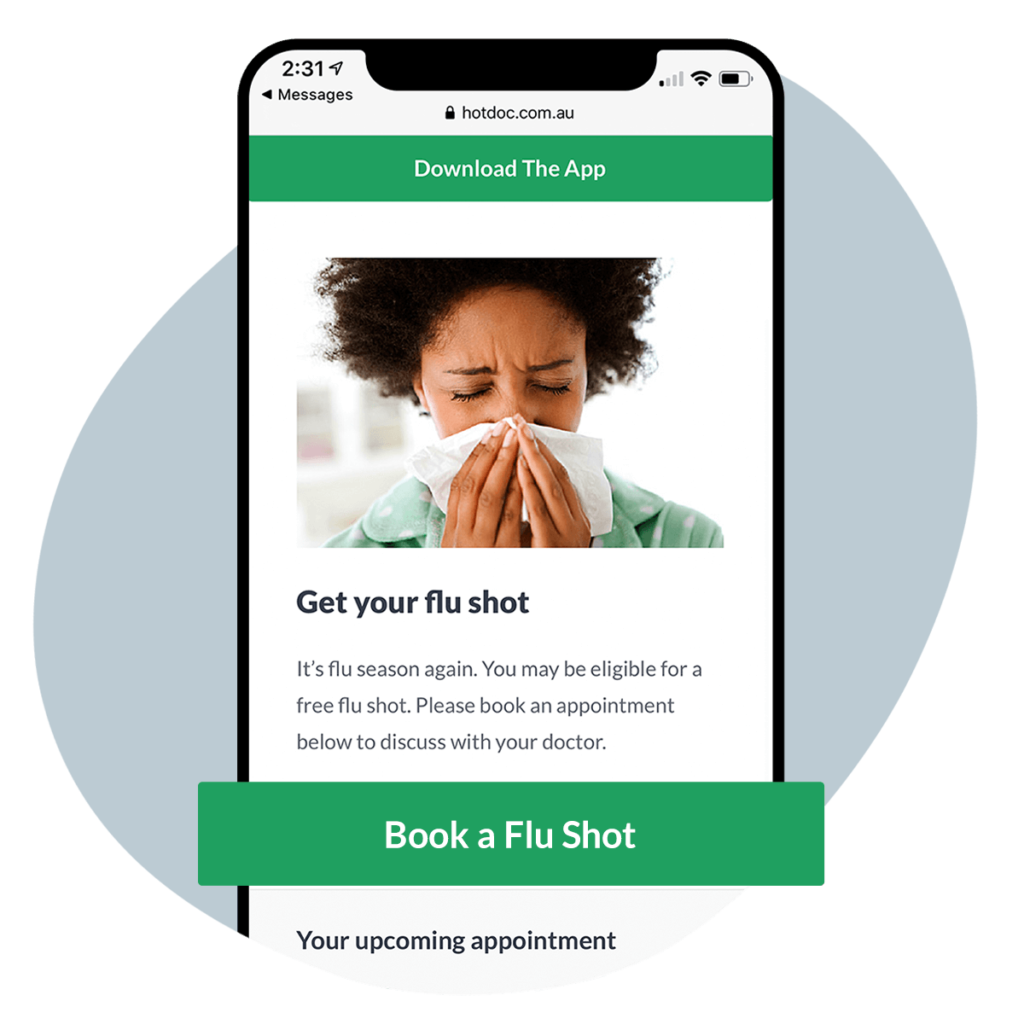
You may also want to consider using HotDoc’s Inform tool. The tool lets you display educational preventative health messages to patients at the time they make an online booking, confirm an SMS appointment reminder, or check-in on their mobile.